Diagnosis of liver disease is a critical step in preventing serious complications such as cirrhosis, liver failure, and liver cancer. Because the liver can continue functioning even when damaged, many people live with liver disease for years without obvious symptoms. This makes proper diagnosis extremely important.
Liver disease diagnosis involves a combination of medical history, physical examination, blood tests, imaging studies, and sometimes liver biopsy. No single test can diagnose all liver conditions, so doctors use multiple tools together.
Early diagnosis allows lifestyle changes and treatment to slow or even reverse liver damage. Late diagnosis often means irreversible scarring has already occurred.
This guide explains all diagnostic methods in simple language so the general public can understand what each test means and why it matters.
This article is part of our complete guide on
Liver Disease: Symptoms, Causes, Diagnosis, Treatment & Prevention
.
When Doctors Suspect Liver Disease
Doctors may suspect liver disease based on symptoms, abnormal blood tests, or risk factors such as obesity, alcohol use, or viral exposure. Often, liver disease is discovered accidentally during routine health checkups.
Mild symptoms such as fatigue or digestive discomfort may not immediately suggest liver problems. However, doctors look for patterns that indicate liver stress.
A detailed medical history helps identify potential causes including medications, alcohol intake, family history, and lifestyle habits.
Once suspicion arises, doctors begin systematic testing to confirm or rule out liver disease.
- Persistent fatigue combined with abnormal blood results raises concern for liver dysfunction. Doctors evaluate how long symptoms have been present. Chronic symptoms often indicate long-term disease.
- Risk factors such as obesity, diabetes, or heavy alcohol use significantly increase suspicion. These factors guide further testing decisions. Screening is often recommended.
- Family history of liver disease suggests genetic causes. Doctors may order specialized tests early. Early detection improves outcomes.
Physical Examination in Liver Disease Diagnosis
A physical examination provides important clues about liver health. Doctors inspect the skin, eyes, abdomen, and extremities for visible signs of liver dysfunction.
Although physical findings alone cannot confirm liver disease, they help determine severity and urgency.
Advanced liver disease often produces physical changes that are visible during examination.
Physical examination findings guide further diagnostic testing.
- Yellowing of the eyes and skin indicates jaundice. This suggests bilirubin buildup due to impaired liver processing. Jaundice often requires urgent investigation.
- Abdominal swelling may indicate fluid accumulation known as ascites. This occurs in advanced liver disease. Doctors assess severity carefully.
- Swollen legs and spider-like blood vessels suggest chronic liver damage. These signs indicate long-standing disease. Further testing is required.
Blood Tests for Diagnosing Liver Disease
Blood tests are the most common and important tools for diagnosing liver disease. They measure liver enzymes, proteins, and waste products processed by the liver.
Abnormal blood results often appear before symptoms develop. This allows early detection.
Doctors interpret blood tests together rather than relying on a single value.
Repeated testing helps monitor disease progression or recovery.
- Elevated ALT and AST enzymes indicate liver cell injury. Higher levels suggest active inflammation. Persistent elevation requires further evaluation.
- Bilirubin levels show how well the liver removes waste. High bilirubin causes jaundice. It indicates impaired liver function.
- Albumin and clotting tests assess liver synthetic ability. Low levels indicate advanced disease. These tests help assess severity.
Imaging Tests Used in Liver Diagnosis
Imaging tests allow doctors to see the liver’s size, shape, and structure. These tests help detect fat accumulation, tumors, scarring, and bile duct problems.
Imaging is painless and non-invasive in most cases.
Different imaging methods provide different types of information.
Imaging helps guide treatment and further testing.
- Ultrasound is the first-line imaging test. It detects fatty liver, tumors, and fluid buildup. It is safe and widely available.
- CT scans provide detailed cross-section images. They help identify tumors and structural abnormalities. Contrast enhances accuracy.
- MRI offers high-resolution images of liver tissue. It is especially useful for detecting early tumors. MRI is highly sensitive.
Liver Biopsy: When Is It Needed?
A liver biopsy involves removing a small tissue sample for microscopic examination. It provides the most accurate information about liver inflammation and scarring.
Biopsy is usually performed when other tests are inconclusive.
The procedure is generally safe but invasive.
Doctors carefully weigh benefits and risks before recommending biopsy.
- Biopsy confirms diagnosis when imaging and blood tests disagree. It provides direct tissue evidence. Accuracy is very high.
- It determines disease stage and fibrosis severity. This guides treatment decisions. Staging affects prognosis.
- Biopsy helps identify specific causes such as autoimmune or genetic disease. This allows targeted therapy. Early diagnosis improves outcomes.
FAQs: Diagnosis of Liver Disease
How is liver disease usually diagnosed?
Liver disease is diagnosed using blood tests, imaging studies, physical examination, and sometimes liver biopsy.
Can liver disease be detected early?
Yes, routine blood tests can detect liver disease before symptoms appear.
Are liver tests painful?
Most liver tests are painless, except biopsy which involves minor discomfort.
What blood tests show liver damage?
ALT, AST, bilirubin, albumin, and clotting tests indicate liver health.
Is ultrasound enough to diagnose liver disease?
Ultrasound helps but cannot confirm all liver conditions alone.
When is a liver biopsy required?
A biopsy is used when diagnosis remains unclear after other tests.
Can liver disease be missed on tests?
Yes, early disease may show mild changes. Repeat testing improves detection.
Do normal liver tests mean healthy liver?
Not always. Some liver diseases show normal tests early.
How often should liver tests be repeated?
Frequency depends on risk factors and medical advice.
Can imaging replace biopsy?
Imaging reduces biopsy need but cannot fully replace it.
Advanced Diagnostic Tests for Liver Disease
When basic blood tests and imaging suggest liver abnormalities, doctors often recommend advanced diagnostic tools to better understand the extent of damage. These tests help measure liver stiffness, inflammation, and scarring without immediately resorting to invasive procedures.
Advanced tests are especially useful for monitoring chronic liver diseases such as fatty liver disease, hepatitis, and early cirrhosis. They allow doctors to track disease progression over time.
Many modern diagnostic tools are non-invasive and can be repeated safely. This makes long-term monitoring more convenient and safer for patients.
Understanding these tests helps patients make informed decisions and reduces anxiety about the diagnostic process.
- Transient elastography measures liver stiffness to assess fibrosis. Increased stiffness suggests scarring. This test is quick, painless, and widely used.
- Serum fibrosis markers use blood samples to estimate scarring levels. These markers help avoid unnecessary biopsies. They are often combined with imaging.
- Specialized panels such as FibroTest evaluate multiple liver parameters. They provide a fibrosis score. Doctors use them for disease staging.
Elastography and Liver Stiffness Measurement
Elastography is an advanced imaging technique that measures how stiff the liver tissue is. Healthy liver tissue is soft, while scarred tissue becomes stiff. This stiffness correlates with fibrosis severity.
This test has become a standard tool for diagnosing and monitoring chronic liver diseases. It is particularly helpful in fatty liver disease and viral hepatitis.
Elastography is non-invasive and can be performed in minutes. No needles or anesthesia are required.
Results help doctors decide whether treatment is needed and how aggressive it should be.
- FibroScan is the most commonly used elastography method. It provides instant stiffness readings. Results are easy to interpret.
- Magnetic resonance elastography offers highly accurate stiffness mapping. It is used in complex cases. This method is more expensive.
- Elastography reduces the need for liver biopsy. It allows frequent monitoring. Patients benefit from less risk.
Diagnosing Fatty Liver Disease
Fatty liver disease is one of the most common liver conditions worldwide. Diagnosis focuses on detecting excess fat in liver cells and identifying inflammation or fibrosis.
Many people with fatty liver disease have no symptoms. Diagnosis often occurs during routine health screenings.
Early diagnosis allows lifestyle changes that may reverse the condition completely.
Advanced stages require close medical monitoring to prevent progression to cirrhosis.
- Ultrasound detects fat accumulation in liver tissue. It is usually the first diagnostic step. Mild cases may be missed.
- Blood tests assess liver inflammation and metabolic risk. Elevated enzymes raise suspicion. Results guide further testing.
- Elastography evaluates fibrosis severity. It helps distinguish simple fatty liver from advanced disease. Treatment plans depend on staging.
Diagnosing Viral Hepatitis
Viral hepatitis is diagnosed using specific blood tests that detect viral antigens, antibodies, and genetic material. These tests determine both infection type and stage.
Early detection of viral hepatitis is crucial to prevent long-term liver damage. Many infections remain silent for years.
Diagnosis also involves assessing liver damage severity through enzyme levels and imaging.
Treatment decisions depend heavily on diagnostic results.
- Hepatitis B and C tests detect viral markers in blood. These confirm active infection. Follow-up tests determine chronicity.
- Viral load testing measures virus quantity. Higher levels indicate active replication. This guides treatment urgency.
- Liver imaging evaluates damage extent. Fibrosis assessment is essential. Early treatment improves outcomes.
Diagnosing Autoimmune and Genetic Liver Diseases
Some liver diseases occur due to immune system malfunction or inherited genetic conditions. These diseases require specialized diagnostic testing.
Autoimmune liver diseases occur when the immune system attacks liver cells. Early diagnosis prevents irreversible damage.
Genetic liver diseases often present early in life but may be diagnosed later due to mild symptoms.
Accurate diagnosis allows targeted treatment and family screening.
- Autoimmune markers in blood confirm immune-related liver damage. These tests are highly specific. Diagnosis requires careful interpretation.
- Genetic tests identify inherited disorders. Early diagnosis improves long-term outcomes. Family members may require testing.
- Liver biopsy confirms diagnosis when blood tests are unclear. It assesses inflammation patterns. Treatment depends on findings.
Monitoring and Follow-Up After Diagnosis
Once liver disease is diagnosed, ongoing monitoring is essential. Regular follow-up helps assess treatment response and disease progression.
Monitoring schedules depend on disease type and severity. Stable patients may need less frequent testing.
Early detection of complications improves survival and quality of life.
Patients play an active role by attending follow-up appointments and adopting healthy habits.
- Regular blood tests monitor liver enzymes and function. Changes indicate improvement or worsening. Adjustments are made accordingly.
- Imaging tests detect complications such as tumors. Early detection saves lives. Screening intervals are important.
- Lifestyle monitoring supports long-term liver health. Diet and exercise are critical. Patient education is essential.
When to See a Liver Specialist
Not all liver conditions require specialist care, but certain situations demand expert evaluation. Early referral can prevent serious complications.
Specialists provide advanced diagnostics and treatment options not available in primary care.
Patients with complex or progressive disease benefit most from specialist care.
Knowing when to seek help improves outcomes.
- Persistent abnormal liver tests require specialist review. Delays worsen outcomes. Early referral is beneficial.
- Signs of advanced disease such as jaundice or ascites need urgent care. These indicate severe damage. Specialist management is required.
- Unclear diagnosis warrants expert evaluation. Advanced tests may be needed. Accurate diagnosis guides treatment.
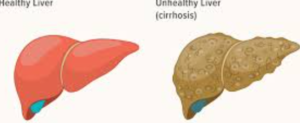
Diagnosing Cirrhosis of the Liver
Cirrhosis is the advanced stage of chronic liver disease, where normal liver tissue is replaced by scar tissue. Diagnosing cirrhosis early is vital because damage at this stage is often irreversible, but complications can still be prevented or delayed.
In many cases, cirrhosis develops silently over years. Patients may only be diagnosed after routine tests show abnormalities or when complications arise.
Doctors use a combination of blood tests, imaging, elastography, and sometimes biopsy to confirm cirrhosis.
Once diagnosed, patients require lifelong monitoring and specialist care.
- Blood tests may show low platelets and impaired clotting. These findings suggest advanced scarring. They help assess severity.
- Imaging reveals a shrunken or nodular liver. Ultrasound and CT scans are commonly used. Structural changes confirm suspicion.
- Elastography provides stiffness scores consistent with cirrhosis. This often replaces biopsy. It is safer and repeatable.
Diagnosis of Liver Cancer in Chronic Liver Disease
People with chronic liver disease are at increased risk of developing liver cancer, especially hepatocellular carcinoma. Early diagnosis significantly improves survival.
Liver cancer screening is recommended for high-risk patients even if they feel well. Screening allows detection at treatable stages.
Doctors use imaging and blood markers together to identify suspicious lesions.
Confirmation often requires advanced imaging rather than biopsy.
- Ultrasound screening every six months detects early tumors. This is standard care for cirrhosis patients. Consistency is critical.
- AFP blood testing helps support diagnosis. Elevated levels suggest malignancy. AFP alone is not definitive.
- CT or MRI confirms tumor characteristics. Imaging patterns are diagnostic. Biopsy is often avoided.
Diagnosis of Liver Disease in Children
Liver disease in children differs from adults in causes, symptoms, and diagnosis. Early identification is especially important to support normal growth and development.
Children may present with poor growth, abdominal swelling, or prolonged jaundice. These signs require immediate evaluation.
Pediatric liver specialists use age-specific tests to determine the cause.
Early diagnosis often leads to better long-term outcomes.
- Blood tests assess liver enzymes and metabolic markers. Results vary by age. Pediatric reference ranges are essential.
- Imaging detects structural abnormalities. Ultrasound is commonly used. It avoids radiation exposure.
- Genetic testing identifies inherited disorders. Early detection allows timely intervention. Family counseling may be required.
Diagnosis of Liver Disease in Older Adults
Diagnosing liver disease in older adults can be challenging because symptoms often overlap with aging or other chronic conditions. Careful evaluation is required.
Medications commonly used by older adults may also affect liver function. Doctors must review drug history carefully.
Age-related changes in liver blood flow can alter test results.
Individualized assessment improves diagnostic accuracy.
- Medication-related liver injury is common. Doctors evaluate drug interactions. Adjustments may be needed.
- Blood test interpretation requires caution. Mild abnormalities may still indicate disease. Trends are important.
- Imaging helps distinguish liver disease from age-related changes. Repeat monitoring improves detection.
Common Diagnostic Errors and Misdiagnosis
Liver disease can be misdiagnosed or missed entirely, especially in early stages. Awareness of common errors helps improve accuracy.
Relying on a single test often leads to incomplete diagnosis. Comprehensive evaluation is essential.
Patients should understand that normal tests do not always mean a healthy liver.
Second opinions are valuable when diagnosis is unclear.
- Ignoring mild enzyme elevation delays diagnosis. Persistent changes require investigation. Follow-up is essential.
- Overlooking risk factors leads to missed screening. Lifestyle history matters. Early testing saves lives.
- Delayed referral to specialists worsens outcomes. Early expert input improves accuracy.
Conclusion: Importance of Early and Accurate Diagnosis
Diagnosing liver disease accurately and early can save lives. Many liver conditions are reversible or manageable when detected in time.
Modern diagnostic tools allow non-invasive assessment and long-term monitoring. Patients should not ignore abnormal results.
Regular screening for at-risk individuals is essential for preventing complications such as cirrhosis and liver cancer.
Awareness, education, and proactive healthcare are key to protecting liver health.