Introduction
Treatment and prevention of liver disease depend on identifying the underlying cause and stopping further liver damage as early as possible. The liver has a unique ability to heal itself, but this ability decreases once damage becomes severe or long-lasting.
Millions of people worldwide live with liver disease without realizing it. Early treatment can reverse many conditions, while delayed care may lead to cirrhosis, liver failure, or liver cancer.
This guide explains all treatment options and prevention strategies in clear, simple language so the general public can understand and take action.
Whether liver disease is caused by lifestyle, infection, genetics, or medication, proper treatment and prevention can significantly improve quality of life.
This article is part of our complete guide on
Liver Disease: Symptoms, Causes, Diagnosis, Treatment & Prevention
.
Goals of Liver Disease Treatment
The primary goal of liver disease treatment is to stop further damage and support the liver’s natural healing process. Treatment plans vary depending on disease type and stage.
Doctors focus on removing harmful factors, treating infections, managing symptoms, and preventing complications.
In early stages, lifestyle changes alone may be sufficient. Advanced disease often requires medications or specialized care.
Understanding treatment goals helps patients stay motivated and compliant.
- Stop progression of liver damage by removing the cause. This includes alcohol cessation or infection treatment. Early action improves outcomes.
- Reduce liver inflammation and scarring. Medications and diet play a key role. Slower scarring means better survival.
- Prevent complications such as cirrhosis or cancer. Regular monitoring supports early intervention. Prevention is always better than cure.
Lifestyle Changes for Treating Liver Disease
Lifestyle modification is the foundation of liver disease treatment. In many cases, changing daily habits can completely reverse early liver damage.
Doctors emphasize lifestyle changes before prescribing medications, especially for fatty liver disease.
These changes require long-term commitment and consistency.
Small improvements can lead to significant liver recovery.
- Complete avoidance of alcohol is critical. Alcohol worsens liver inflammation and scarring. Even small amounts can be harmful.
- Weight loss improves fatty liver disease. Losing 5–10% of body weight reduces liver fat. Sustainable methods work best.
- Regular physical activity boosts liver metabolism. Exercise reduces fat buildup. Consistency matters more than intensity.
Dietary Treatment for Liver Disease
Diet plays a powerful role in both treating and preventing liver disease. The liver processes nutrients, fats, and sugars, making food choices extremely important.
A liver-friendly diet reduces fat accumulation and inflammation.
Poor diet accelerates disease progression even with medication.
Dietary guidance should be personalized when possible.
- High-fiber foods support liver detoxification. Fruits, vegetables, and whole grains are essential. Fiber improves insulin sensitivity.
- Reducing sugar and refined carbs lowers liver fat. Sugary drinks are especially harmful. Small reductions make big differences.
- Healthy fats improve liver function. Olive oil and nuts are beneficial. Trans fats should be avoided.
Medical Treatment Based on Liver Disease Cause
Medical treatment depends on what caused liver disease. Different conditions require different therapeutic approaches.
Doctors aim to treat the root cause rather than symptoms alone.
Medication effectiveness increases when combined with lifestyle changes.
Regular monitoring ensures treatment safety.
- Antiviral medications treat hepatitis B and C. These drugs suppress or eliminate the virus. Early treatment prevents cirrhosis.
- Immunosuppressive drugs manage autoimmune liver disease. They reduce immune attacks on liver cells. Long-term follow-up is required.
- Medication adjustment treats drug-induced liver injury. Stopping the harmful drug allows recovery. Doctors monitor improvement closely.
Preventing Progression to Cirrhosis
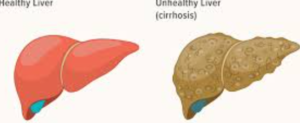
Preventing cirrhosis is a key goal in liver disease management. Once cirrhosis develops, damage is usually permanent.
Early-stage liver disease offers a critical window for prevention.
Monitoring and compliance are essential.
Patient education plays a major role.
- Regular liver function tests track disease progression. Early changes prompt intervention. Monitoring saves lives.
- Avoiding liver toxins prevents further scarring. Alcohol and unnecessary drugs must be avoided. Safety awareness is crucial.
- Managing diabetes and cholesterol protects the liver. Metabolic control reduces inflammation. Whole-body health matters.
Treatment of Advanced Liver Disease and Cirrhosis
When liver disease progresses to advanced stages or cirrhosis, treatment focuses on slowing further damage, managing symptoms, and preventing life-threatening complications. Although cirrhosis damage is usually permanent, proper care can significantly extend life expectancy.
Patients with cirrhosis require close medical supervision. Treatment plans are often individualized based on disease severity and underlying cause.
Lifestyle changes remain important even in advanced disease. Medications and procedures are added as needed.
Early management of complications improves survival and quality of life.
- Medications reduce portal hypertension and fluid buildup. These drugs lower pressure in liver blood vessels. Proper dosing is critical.
- Diuretics help manage ascites and swelling. Salt restriction improves effectiveness. Patients require regular monitoring.
- Nutritional support prevents muscle wasting. Protein intake is adjusted carefully. Dietitian guidance is beneficial.
Managing Complications of Liver Disease
Complications of liver disease arise when the liver can no longer perform essential functions. Managing these complications is a major part of treatment.
Early recognition of complications prevents emergency situations.
Patients and caregivers should understand warning signs.
Regular follow-up allows timely intervention.
- Hepatic encephalopathy is treated with medications that reduce toxins. Mental clarity often improves. Adherence is essential.
- Variceal bleeding is prevented using medications and endoscopic procedures. Early screening saves lives. Emergency care may be needed.
- Infections are treated aggressively due to weakened immunity. Vaccination reduces risk. Prompt treatment prevents complications.
Treatment of Fatty Liver Disease
Fatty liver disease is one of the most treatable forms of liver disease when addressed early. Treatment focuses primarily on lifestyle changes rather than medication.
Weight loss and metabolic control are the most effective treatments.
Even modest improvements can significantly reduce liver fat.
Ongoing monitoring ensures disease reversal.
- Gradual weight loss reduces liver fat safely. Crash diets are harmful. Sustainable changes are recommended.
- Blood sugar control prevents disease progression. Diabetes management is essential. Medication adjustments may help.
- Exercise improves liver insulin sensitivity. Aerobic and resistance training are beneficial. Consistency is key.
Preventing Liver Cancer in Chronic Liver Disease
People with chronic liver disease face a higher risk of developing liver cancer. Prevention and early detection greatly improve survival.
Cancer prevention strategies focus on controlling liver inflammation and scarring.
Routine screening is essential for high-risk individuals.
Education helps patients understand the importance of monitoring.
- Antiviral therapy reduces cancer risk in hepatitis patients. Viral suppression protects liver cells. Early treatment is best.
- Ultrasound screening every six months detects early tumors. Early treatment improves survival. Consistency is vital.
- Avoiding alcohol and toxins lowers cancer risk. Liver protection is lifelong. Prevention is cost-effective.
Vaccination and Infection Prevention
Preventing liver infections is a key component of liver disease prevention. Vaccination and hygiene play critical roles.
People with liver disease are more vulnerable to infections.
Preventive care reduces hospitalizations and complications.
Public awareness improves vaccination rates.
- Hepatitis A and B vaccines prevent viral liver infections. Vaccination is safe and effective. High-risk groups benefit most.
- Safe food and water practices prevent hepatitis A. Hygiene reduces transmission. Education is essential.
- Avoiding shared needles prevents hepatitis transmission. Harm-reduction strategies save lives. Community programs help.
Liver Transplant: When Treatment Options Are Limited
A liver transplant becomes necessary when severe liver disease progresses to end-stage liver failure and no other treatments can restore liver function. Transplantation replaces the diseased liver with a healthy donor liver.
Modern transplant medicine has greatly improved survival rates. Many patients live long, healthy lives after transplantation with proper care.
Eligibility for transplant depends on disease severity, overall health, and absence of contraindications.
Post-transplant care requires lifelong monitoring and medication adherence.
- Transplant evaluation includes blood tests, imaging, and cardiac assessment. This ensures patient readiness. Careful selection improves outcomes.
- Immunosuppressive medications prevent organ rejection. These must be taken for life. Regular monitoring reduces side effects.
- Lifestyle changes remain essential after transplant. Healthy habits protect the new liver. Long-term success depends on compliance.
Long-Term Prevention Strategies for Liver Health
Preventing liver disease is more effective and less costly than treating advanced illness. Long-term prevention requires awareness, education, and consistent healthy behaviors.
Even people without diagnosed liver disease should adopt liver-protective habits.
Small daily choices significantly impact liver health over time.
Prevention strategies benefit overall health as well.
- Limiting alcohol intake prevents liver inflammation. Abstinence is safest for high-risk individuals. Moderation reduces long-term risk.
- Maintaining a healthy weight protects against fatty liver disease. Balanced diet and exercise are key. Consistency matters.
- Avoiding unnecessary medications reduces liver strain. Always consult healthcare providers. Safe use prevents injury.
Screening and Public Health Measures
Public health initiatives play a crucial role in reducing liver disease burden. Screening and education help detect disease early.
High-risk populations benefit most from routine screening programs.
Early detection reduces healthcare costs and saves lives.
Community awareness strengthens prevention efforts.
- Screening for hepatitis B and C identifies silent infections. Early treatment prevents complications. Public programs increase access.
- Fatty liver screening in people with obesity or diabetes detects disease early. Lifestyle changes are most effective then.
- Education campaigns promote vaccination and safe practices. Awareness reduces transmission. Prevention benefits society.
Frequently Asked Questions (FAQs)
Can liver disease be cured?
Some liver diseases can be reversed if treated early, while advanced disease can often be managed but not cured.
What is the best treatment for fatty liver disease?
Weight loss, healthy diet, and regular exercise are the most effective treatments for fatty liver disease.
Is alcohol completely banned in liver disease?
Yes, alcohol should be completely avoided in most liver diseases to prevent further damage.
Can medications damage the liver?
Yes, some medications can cause liver injury, especially when misused or combined with alcohol.
How can liver disease be prevented?
Healthy lifestyle, vaccination, safe medication use, and regular screening prevent liver disease.
When is liver transplant needed?
A liver transplant is needed in end-stage liver failure when other treatments no longer work.
Can liver disease come back after treatment?
Yes, liver disease can return if risk factors are not controlled or treatment is stopped.
Does diet alone heal the liver?
Diet helps significantly but may not be sufficient alone in advanced disease.
Are herbal supplements safe for liver health?
Some supplements can harm the liver. Always consult a healthcare provider before use.
How often should liver tests be repeated?
Testing frequency depends on disease severity and doctor recommendation.
Conclusion: Protecting Your Liver for Life
Liver disease is largely preventable and manageable when detected early. Treatment success depends on timely medical care, healthy lifestyle choices, and long-term commitment.
Modern medicine offers effective therapies, but prevention remains the strongest defense against liver disease.
Regular screening, vaccination, and education empower individuals to protect their liver health.
By taking proactive steps today, you can safeguard your liver for the future.